Preservatives in eye drops should be avoided as they may worsen the patient’s condition. This applies particularly to patients with moderate and severe dry eye, who may have to use eye drops quite frequently.
In 2007, the DEWS1 report stated clearly that “Many components of eye drop formulations can induce a toxic response from the ocular surface. Of these, the most common offenders are preservatives, such as benzalkonium chloride (BAC), which cause surface epithelial cell damage and punctuate epithelial keratitis, which interferes with surface wettability. Use of preserved drops is an important cause of dry eye signs and symptoms in glaucoma patients, and it is usually reversible on switching to non-preserved preparations. Therefore, frequent applications of preserved artificial tear preparations should be avoided
The new DEWSII report issued in July 2017 has this to say about preservatives: “Chronic exposure of the ocular surface to preservatives is now well recognized to induce toxicity and adverse changes to the ocular surface…preservative-free drops may be a better choice for patients who have pre-existing ocular surface conditions and/or need frequent instillation of eye drops…. Preservative-free eye drops have shown greater effectiveness than preserved drops in decreasing inflammation on the ocular surface and increasing the antioxidant contents in tears of patients with DED.”
Recent progress in the mechanisms of toxic reaction of preservatives
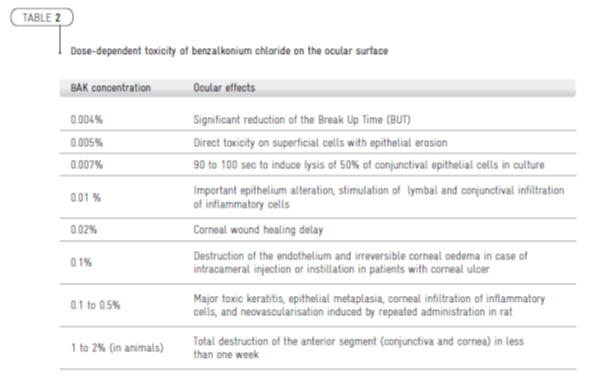
The mechanisms of preservative toxicity are still not fully elucidated, but significant progress has been performed since two decades of research. It is now well established that benzalkonium chloride (BAK) exerts significant toxic, pro-oxidative, pro-apoptotic, and pro-inflammatory activity on exposed cells or tissues. Three mechanisms of BAK toxicity have been described [6]: detergent effect, causing loss of tear film stability; direct damages to the corneal and conjunctival epithelium; immunoallergic reactions. As summarised in Table 1, BAK in case of glaucoma medication can cause tear film instability, goblet cell loss, conjunctival squamous metaplasia and apoptosis, disruption of the corneal epithelial barriers, and damages to deeper ocular tissues [3].
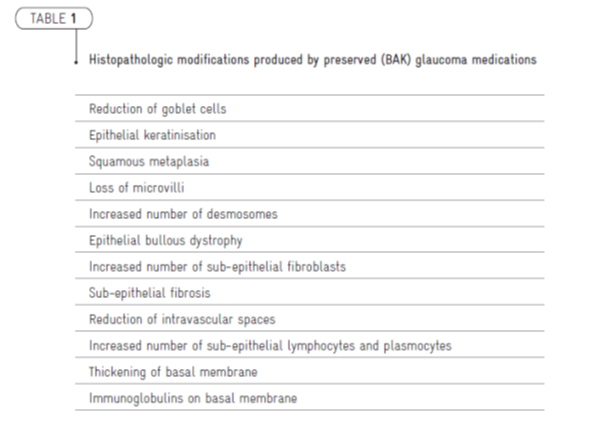
One of most important progress in preservative research was the confirmation using sensitive and non invasive technics (including in vivo confocal microscopy) that preservatives may exert their toxicity at low concentrations and at a subclinical level. It was evidenced that not only the ocular surface but also deep ocular structures, including the trabeculum, may be affected (Table 2). Other data from numerous studies suggest that adverse effects of preserved ocular medication may occur following a cumulative process involving a long, dose-dependent and time-dependent exposure.