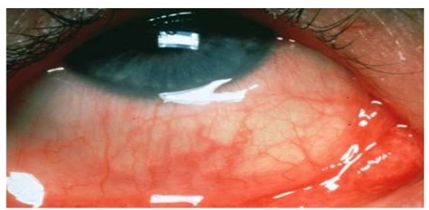
Allergic conjunctivitis is an inflammatory response of the conjunctiva to an allergen. It is part of a larger systemic atopic reaction and is usually seasonal with associated upper respiratory tract symptoms and complaints of redness and swelling of the conjunctiva with severe itching and increased lacrimation. Presence of rhinitis often terms this process as allergic rhinoconjunctivitis
Classification
- Vernal – of, or appropriate to spring
- Atopic – denoting a form of allergy or hypersensitivity reaction
- Perennial – chronic, year round
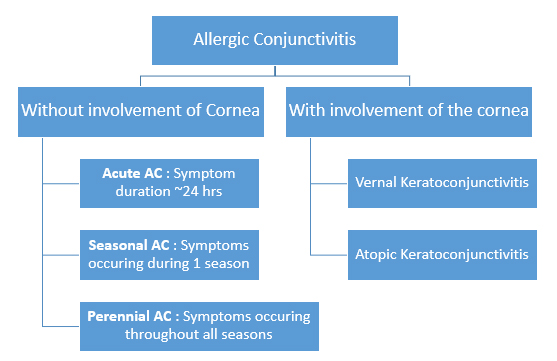
| Grouping | Type | Risk Factors |
| Without corneal involvement | Acute | Environmental allergens, particularly if they are known; an example is cat dander. |
| Seasonal | Environmental allergens that are often associated with changes in seasons; examples include grass and weed pollens. | |
| Perennial | Environmental allergens that occur throughout the year; examples include Indoor allergens: dust mites, mold, animal dander. | |
| With corneal involvement | Vernal | Environmental allergens may incite an acute exacerbation. Most commonly present during the springtime with the associated increase in pollen. Increased presence in hot and dry environments with a decrease in inflammation and symptoms during the winter months. |
| Atopic | Genetic predisposition to atopic reactions with comorbid asthma and atopic dermatitis commonly present. Increased risk with positive family history. Environmental allergens may cause an acute exacerbation as well. No changes with seasons. | |
| Giant papillary conjunctivitis (GPC) | Commonly seen in individuals wearing soft contact lens who infrequently replace their lenses, wear their lenses for prolonged periods of time, have poor lens hygiene, have poor contact lens fitting, or are allergic to the various contact lens solution. Similarly, irritation from exposed sutures or prostheses increase the risk for developing GPC. | |
| solution. Similarly, irritation from exposed sutures or prostheses increase the risk for developing GPC. |
Signs & Symptoms
- Swelling or puffiness of the eyes
- Redness
- Itching
- Tearing
- Mucous discharge
Physical Examination:
| Type of Allergic Conjunctivitis | Physical Exam Findings |
| Seasonal/Perennial conjunctivitis | Bilateral conjunctival injection, chemosis, watery discharge, and mild mucous discharge. |
| Vernal keratoconjunctivitis (VKC) | Bilateral bulbar conjunctival injection with associated watery and mucoid discharge. Patients develop a giant papillary hypertrophy of only the superior tarsal conjunctiva, resembling “cobblestones”. Specific findings that help differentiate VKC from AKC are: limbal (Horner-Trantas) dots which are small white-yellow chalky concretions around the corneal limbus; corneal vernal plaques; or shield (Togby’s) shaped ulcers of the cornea. Just as in AKC, patients, if untreated, can develop conjunctival scarring or corneal neovascularization, scarring, or erosions/ulcers. |
| Atopic keratoconjunctivits (AKC) | Bilateral conjunctival injection with associated eczematoid belpharitis, watery/mucoid discharge, and boggy edema. Papillary hypertrophy of superior or inferior tarsal conjunctival can occur with increased risk for eyelid thickening and scarring. In more severe and untreated cases, patients can develop loss of eyelashes, conjunctival scarring, corneal neovascularization, ulcers or scars, punctate epithelial keratitis and associated keratoconus and/or anterior/posterior subcapsular cataracts. |
| Giant papillary conjunctivitis (GPC) | The laterality of symptoms is associated with contact lens, suture, or prostheses wear pattern. Most notably, patients will have papillary hypertrophy of the superior tarsal conjunctiva. In long-standing, untreated disease, the papillae will develop white fibrotic centers. In severe cases, patients will have lid swelling and ptosis. |
- First line: Over-the-counter antihistamine/vasoconstrictor agent. Vasoconstrictors: Inexpensive over-the counter are first line. Many brands are available containing antazoline phosphate 0.05%, naphazoline HCl 0.05%, oxymetazoline HCl, tetrahydrozoline HCl 0.05%, or phenylephrine 0.12%.
- Second line: Second-generation topical histamine H1-receptor antagonist. H-1 receptor antagonists: More effective than the vasoconstrictors, but much more expensive. The three principal choices are pheniramine maleate 0.3% (Naphcon), emedastine (Emadine), and levocabastine HCl 0.05% (Livostin)
- Third line: recurrent/persistent – mast-cell stabilizers can be used. Mast cell stabilizers: cromolyn sodium 4% (Crolom), nedocromil 2% (Alocril), pemirolast 0.1% (Alamast), and lodoxamide tromethamine 0.1% (Alomide). These are FDA-approved only for a specifically vernal conjunctivitis. Use only if other classes of medications have failed.
- Combined medications can also be used: Combined H-1 receptor antagonist and mast cell stabilizers: olopatadine hydrochloride 0.1% (Patanol), optivar, and Elestat. These agents are more effective than the mast cell stabilizers alone.
- If symptoms are not adequately controlled: Brief course of low-potency and low-frequency topical corticosteroids. NSAID such as ketorolac has been approved by FDA for use of seasonal allergic conjunctivitis but are generally used as adjunctive agents. Nonsteroidal anti-inflammatory agents: ketorolac tromethamine 0.5% (Acular) and ketotifen 0.025% (Zaditor).
- Oral antihistamines, such as Xyzal (levocetirizine), Zyrtec (cetirizine), Allegra (fexofenadine), Clarinex (desloratadine) and Clarinex (loratadine), can be used, especially if the patient is experiencing additional systemic effects.
- Some additional measures can be used as adjunctive measures to improve symptom management are as follows:
- Artificial tears to dilute allergens
- Cool compresses / ice packs
- Avoid Allergens
- Frequent clothes washing and bathing/showering before bedtime
- Refer/consult allergy or dermatology for those who are not adequately controlled with topical medications and oral antihistamines