Inflammation is the natural (protective) response of the body towards External Provocative Stimulus-
- Injury / Trauma
- Infection and Allergy
Causes
- Allergy
- Infection
- Trauma ( accident or surgery )
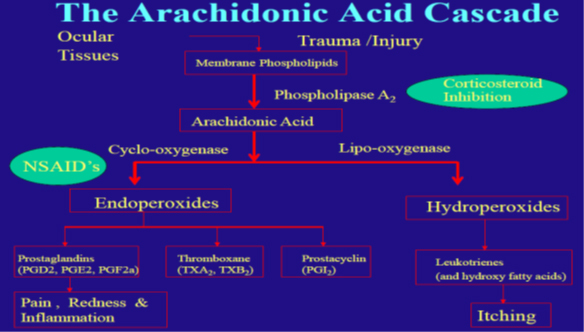
Tissue damage leads to release of membrane phospholipids exposing cell membrane substances to the action of enzymes (Phospholipase A-2)
Arachidonic Acid pathway initiates leading to release of inflammatory mediators.
Types of Inflammatory Mediators:
- Prostaglandins (Arachidonic pathway)
- Leukotrienes ( Arachidonic pathway)
- Histamine ( Mast Cells)
- Kinins (Blood Plasma)
- Serotonin ( Blood Platelets)
- Blepharitis – Inflammation of eyelids.
- Conjunctivitis – Inflammation of conjunctiva.
- Dacryocystitis – Inflammation of lacrimal apparatus.
- Iritis – Inflammation of iris.
- Keratitis – Inflammation of cornea.
- Uveitis – Inflammation of uveal tract.

OCULAR INFLAMMATION TREATMENT
- Ocular steroids
- NSAIDs
OCULAR STEROIDS
“Steroid” is a chemical name for any substance that has a characteristic chemical structure consisting of multiple chemical rings of connected atoms.
- Natural Steroids – Vitamin D, Cholesterol, Estrogen, Progesterone, Cortisol
- Synthetic Steroids – Prednisolone, Dexamethasone, Betamethasone
Adrenal Gland
Two in number, superior and slight medial to kidneys
2 parts : Adrenal cortex (80%), Adrenal medulla (20%)
Comprises 3 zones :
- ZONA GLOMERULOSA : Produce mineralocorticoids i.e Aldosterone
- ZONA FASCICULATA : Produce glucocorticoids g Cortisol , corticosterone , small amount of adrenal androgens and estrogens
- ZONA RETICULARIS : Produce androgens e.g Dehydroepiandrosterone ,small amount of estrogen and some glucocorticoids
FUNCTION OF MINERALOCORTICOIDS
- Effect on carbohydrate metabolism- e stimulation of gluconeogenesis
- Effect on protein metabolism – Reduction of cellular protein
- Effect in resisting stress – Almost all type of stress ( trauma , infections , intense heat and cold , surgery ) cause immediate and marked increase adrenocotical secretion of cortisol
- Effect on immunity and blood – Decreases activation and migration of leukocytes, Lyse and destroy lymphocytes
- Effect as strong anti-inflammatory agent
Five different stages of the inflammation :
- Chemicals such as histamine , bradykinin , proteolytic enzymes , prostaglandins and leukotrienes from damage tissue cells activates the inflammation
- Increases blood flow due to vasodilation called erythema
- Leakage of plasma out of capillaries into damaged area because increase capillary permiability
- Infiltration of area by leukocytes
- After few days ingrowth of fibrous tissue that often helps in the healing process
Basic steroidal activities towards inflammation
- Reduce histamine release from basophils induced by IgE dependent stimulus
- Inhibit phospholipase A2 which prevents biosynthesis of arachidonic acid and subsequent formation of prostacyclin, prostaglandins and leukotrienes
- Decrease capillary permeability and fibroblast proliferation and the quantity of collagen deposition thus influencing tissue regeneration and repair
- The anti-inflammatory effects are nonspecific, occurring whether the etiology is allergic, traumatic or infectious
Corticosteroid | Derivative | Formulation | Concentration |
Prednisolone | Acetate | suspension | 0.125% or 1% |
Prednisolone | Sodium phosphate | solution | 0.125% or 1% |
Dexamethasone | Alcohol | Suspension | 0.1 |
Dexamethasone | Sodium phosphate | Solution Ointment | 0.1 0.05 |
Flourometholone | Alcohol | Ointment Suspension | 0.1 0.1 |
Flourometholone | Acetate | Suspension Suspension | 0.25 0.1 |
Prednisolone
- A synthetic analogue of the major glucocorticoid e cortisol or hydrocortisone
- Effective for external as well as intraocular inflammation
- Commercially formulated as acetate and phosphate ; acetate derivative being more effective anti-inflammatory agent
- Not available as an ophthalmic ointment.
Available in concentration of 0.5% and 1% W/V
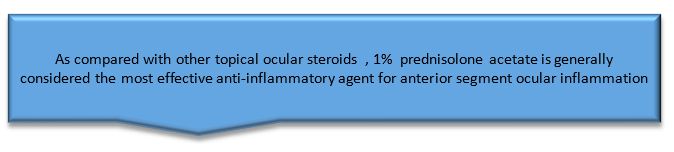
- Prednisolone acetate 1% is considered the standard, by which all other topical ocular corticosteroids are compared
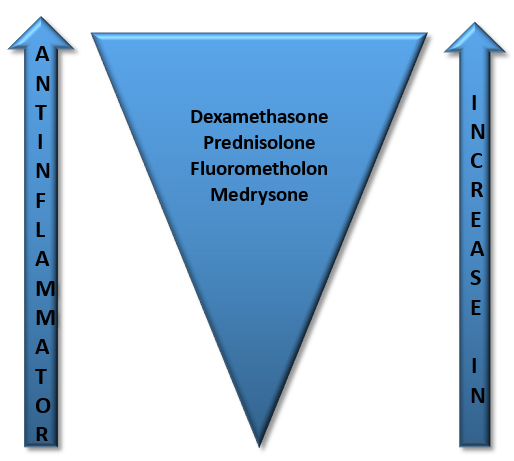
Dexamethasone
- Structurally resemble cortisol
- Available as an alcohol or phosphate derivative
- 1% ophthalmic suspension or solution
- Alcohol derivative more active than phosphate
- Resistant to metabolism after penetration into the aqueous humor.
- Very effective in reducing ocular inflammation
- But has the propensity to increase IOP more than any other topical ophthalmic corticosteroid
- Usually limited to shortcourse therapy
- Dexamethasone ointment is very useful for nighttime coverage in cases of uveitis
Fluorometholone (FML)
- Structurally resemble progesterone
- Formulated both as an alcohol and acetate derivative
- Relatively weaker corticosteroid
- Decreased risk of unwanted complications, such as IOP rise
- Treatment of choice in those patients with a history of pressure rise due to corticosteroid therapy or previously diagnosed glaucoma
- An effective agent in external ocular inflammations , like conjunctivitis, piguiculitis , scleritis and episleritis
- Available as 0.1% drop
Medrysone
- Like fluorometholone , a synthetic derivative of progesterone
- Weakest of the available ophthalmic steroids
- Useful for superficial ocular inflammations , including allergic and atopic conjunctivitis
- Generally do not respond to intraocular inflammatory conditions
- Elevates IOP minimally or not at all
Betamethasone
- Available as 0.1% eyedrop or ointment
- Marked anti-inflammatory action
- Low dose is enough
- So, reduces the risk of side effects
Hydrocortisone
- 1st corticosteroid used in medicine
- Available as 1% eyedrop and 0.5%, 1% or 3% ointment
Rimexolone
- Available as a 1% ophthalmic suspension (Vexol)
- Effective in suppressing cells, flare, keratin precipitates and photophobia
- Main advantage – more of site-specific action than other corticosteroids
- Less tendency to increase the IOP.
LOTEPREDNOL
- Available as 0.2% and 0.5% concentration
- Less potent steroid
- Indicated for temporary relief of the signs and symptoms of seasonal allergic conjunctivitis
BIOAVAILABILITY OF TOPICAL STEROIDS
- Fraction of unchanged drug reaching the systemic circulation
- Depends upon the ability to penetrate cornea
- The ideal steroid should be biphasic i.e solubility in both the lipid (hydrophobic) layers of the epithelium and endothelium and the aqueous (hydrophilic) media of the stroma
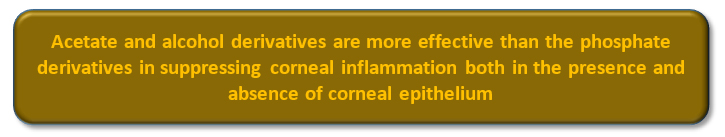
- Acetate and alcohol derivatives more lipophilic i.e fat soluble
- Sodium phosphate and hydrochloride more hydrophilic i.e water soluble
- So, in intact epithelium , penetration of acetate greater while in absence of epithelium penetration of phosphate greater
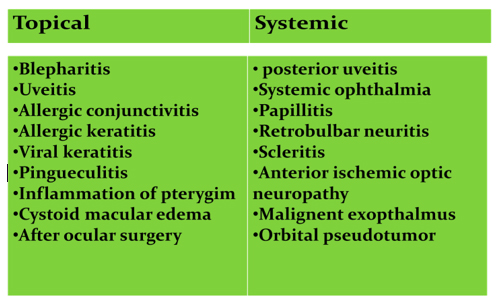
Routes of administration
TOPICAL | SYSTEMIC |
|
|
|
|
|
|
|
|
Ocular indications
Why steroids dozes tapered ??
- Synthetic cortisone medication mimic cortisol,i.e naturally occuring hormone produced by adrenal gland
- Excess production of cortisol – negative feedback mechanism (HPA axis)
- Using large dose for few days or smaller dose for more than two weeks—prolonged decrease in HPA axis function
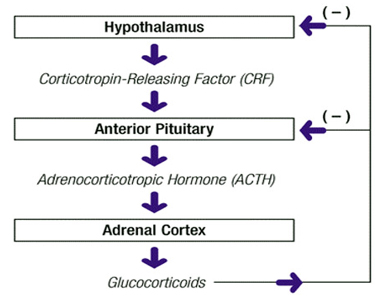
- So tapering is required i.e continuing the therapy for several days in reduced dose
- Gives time for adrenal glands to return their normal patterns of secretion
- Also reduces the chance of recurrence of the disease
Locally (in case of topical) ??
Corticosteroids reduce the leukocyte cells locally
White cells proliferate when therapy stops
Immature cells can produce large quantities of antibodies to residual antigen in the ocular tissue
Massive polymorphonuclear leukocytic reaction follows the resultant antigen- antibody reaction
This sequence of events , unless interrupted immediately , can lead to a recurring , serious necrotizing inflammation
Thus depending upon response and dozes used , topical therapy should generally be tapered over several days to weeks
Removal of corneal epithelium caused appearance of leukocytes in tear fluid within 2-5 hrs which was greatly reduced by 1% prednisolone and 0.01% flurbiprofen
Indications of Steroids
- Eyelids :
- Allergic blepharitis
- Contact dermatitis
- Herpes zoster dermatoblepharitis
- Chemical burns
- Neonatal hemangioma
- Conjunctiva
- Allergic conjunctivitis
- Vernal conjunctivitis
- Herpes zoster conjunctivitis
- Chemical burns
- Mucocutaneous conjunctival lesions
- Cornea
- Immune reaction after keratoplasty
- Herpes zoster keratitis
- Disciform keratitis
- Marginal corneal infiltrates
- Superficial punctate keratitis
- Chemical burns
- Acne rosacea keratitis
- Interstitial keratitis
- Uvea
- Anterior uveitis
- Posterior uveitis
- Sympathetic ophthalmia
- Sclera
- Scleritis
- Episcleritis
- Retina
- Retinal vasculitis
- Optic nerve
- Optic neuritis
- Temporal arteritis (arteretic anterior ischaemic optic neuropathy)
- Globe
- Endophthalmitis (except fungal endopthalmitis
- Hemorrhagic glaucoma
- Orbit
- Pseudotumor
- Graves’ ophthalmopathy
- Extraocular muscles
- Ocular myasthenia gravis
OCULAR SIDE EFFECTS
- Posterior subcapsular cataracts
- Ocular hypertension or glaucoma
- Secondary ocular infection
- Retardation of corneal epithelial healing
- Keratitis
- Corneal thinning or melting
- Scleral thinning
- Uveitis
- Mydriasis
- Ptosis
- Transient ocular discomfort



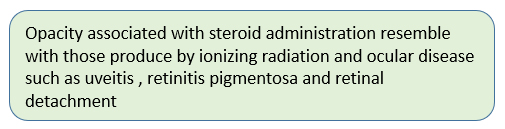
Cataract
- Occurrence of PSCC with all routes
- High incidence found in long term systemic therapy then the topical therapy
Mechanism -1
Glucocorticoids enter lens fibres »
reacts with lens crystallins »
conformational change within cells »
release of sulfhydryl groups »
Form disulfide bonds »
protein aggregation »
CATARACT
Mechanism -2
Corticosteroid induces the production of the new lens fibers through equatorial region »
Which goes and accumulate in posterior sub capsular region »
Finally causes cataract
Ocular hypertension or glaucoma
- Reversible elevation of pressure with repeated use of topical steroids.
- Steroid induced glaucoma ; a form of secondary open-angel glaucoma
How steroids increase IOP…..?
IOP elevation in different steroid
- Dexamethasone 0.1% 0 +/- 2.9
- Prednisolone 1% 0 +/-1.7
- Fluoromethalone 1% 6.1 +/-1.4
- Hydrocortisone 5% 3.2 +/-1.0
- Tetrahydrotriamcenalone 0.25% 8 +/-1.3

- Medrysone 1% 0 +/-1.3
- Individuals differ in their responsiveness: approximately 4% develop pressures higher than 31 mm Hg after 6 weeks of therapy with topical dexamethasone
- Steroid- induce IOP elevation almost never occurs in less than 5 days and rarely in less than 2 weeks
- Steroid-induce IOP rises are usually reversible by discontinuance of therapy if the drug has not been used for more than 1 year , but permanent elevations of pressure are common if the therapy has continued for 18 months or more 1

1 (armaly MF and becker b . Mills DW ARCH OPHTHALMOL 2003)
Ocular NSAIDs
Nepafenac
- Nepafenacis a non-steroidal anti-inflammatory drug (NSAID), usually sold as a prescription eye drop 0.1% solution.
- Nepafenac 0.1% is a sterile, topical, nonsteroidal anti-inflammatory (NSAID) prodrug for ophthalmic use. Each mL of Nepafenac suspension contains 1 mg of nepafenac.
- Nepafenac is manufactured by Alcon and sold under the trade name Nevanac.
- It is used to treat pain and inflammation associated with cataract surgery.
- The usual dose is one drop, thrice a day, in each affected eye beginning one day prior to cataract surgery, continued on the day of surgery and through the first two weeks of the postoperative period.
- Nepafenac is a prodrug of amfenac, an inhibitor of COX-1 and COX-2 activity.
- After topical ocular dosing, nepafenac penetrates the cornea and is converted by ocular tissue hydrolases to amfenac, a nonsteroidal anti-inflammatory drug.
- Amfenac is thought to inhibit the action of prostaglandin H synthase (cyclooxygenase)- , an enzyme required for prostaglandin production.
Ketorolac
- KT-LUME – ketorolac tromethamine ophthalmic solution 0.5% is a member of nonsteroidal anti-inflammatory drugs (NSAIDs) for ophthalmic use.
- ophthalmic solution is supplied as a sterile isotonic aqueous 0.5% solution, with a pH of 7.4.
- Ketorolac tromethamine is a nonsteroidal anti-inflammatory drug which, when administered systemically, has demonstrated analgesic, anti-inflammatory, and anti-pyretic activity. The mechanism of its action is thought to be due to its ability to inhibit prostaglandin biosynthesis.
- KT- LUME ophthalmic solution is indicated for the temporary relief of ocular itching due to seasonal allergic conjunctivitis.
- KT- LUME ophthalmic solution is also indicated for the treatment of postoperative inflammation in patients who have undergone cataract extraction.