Dry eye syndrome is a multifactorial disease of the tears and ocular surface that results in a range of symptoms, including discomfort, visual disturbance, tear film instability and potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface. The Ocular Surface, 2007, pp.77. 2007 Report of the International Dry Eye Workshop (DEWS).
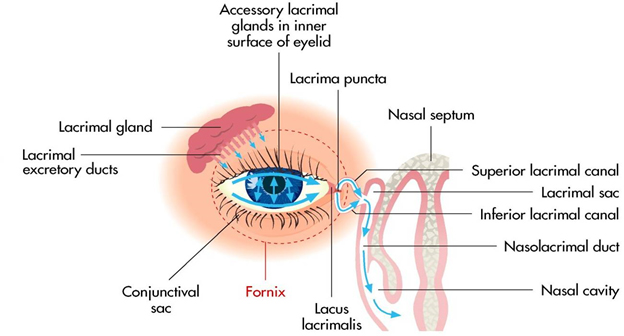
Dry eye syndrome is a disturbance of the Lacrimal Functional Unit, which comprises the lacrimal glands, ocular surface (cornea, conjunctiva and meibomian glands) and eyelids, together with the sensory and motor nerves that link them.
The key features of dry eye syndrome are:
- Decreased tear production
- Increased tear evaporation
- Incorrect composition of tears
These result in inadequate lubrication of the eyes.
Dry eye is a catch-all term referring to abnormalities of the tear layer which normally coats the surfaces of the eyes, providing clear vision and protecting sensitive surface tissues. Other names for dry eye syndrome include chronic dry eye, dry eye disease and keratoconjunctivitis sicca.
What about tears?
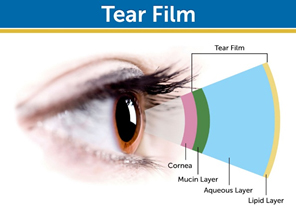
- A sensation of dryness happens whenever the tear film becomes destabilized, breaks down and thus no longer lubricates the eye sufficiently. The tear film is a complex structure and has various functions:
- It lubricates the surface of the eye
- It keeps the surface tissue of the eye moist
- It supplies nutrients and oxygen to the cornea
- It hinders bacterial infections
- It protects the eye from small dust particles
How dry eye develops?
Mucus-secreting cells create the mucin layer. Mucus coats the cornea and protects the surface.
The superficial lipid layer of the tear film is derived from the meibomian glands, embedded within the eyelids. The gland ducts open on the eyelid margin. The lipid layer serves to reduce evaporation of underlying aqueous fluid in the open eye. Abnormalities in the secreted lipids result in increased evaporation of tears.
The aqueous layer of the tear film is produced by the lacrimal gland, beneath the upper eyelid. This layer provides moisture, oxygen and electrolytes to the cornea. The concentration of the aqueous layer increases as a result of dry eye and can lead to increased tear osmolarity. In severe dry eyes the tear hypertonicity has been shown to cause ocular surface disease.
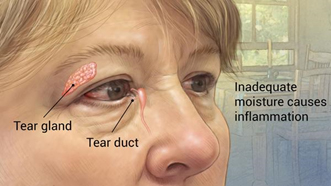
Eye surface inflammation is the key mechanism of ocular surface injury in dry eye and results in further cell damage. Inflammation may be initiated by dryness, hypertonicity of tears, microtrauma from eyelids, proinflammatory substances released by the lacrimal glands and a reduced supply of supportive factors from tears. Inflammation is enhanced by cytokines secreted by damaged surface epithelial cells and lymphocytes and leukocytes that leak out from dilated conjunctival blood vessels. Ocular surface inflammation reduces surface wettability and tear film stability. (Prog Retin Eye Res. 2004 Jul; 23(4):449-74)
Symptoms
Patients will present with some or all of the following symptoms:
- Feeling like there is something in their eye (foreign body sensation)
- Scratchy, gritty eyes
- Aching or sore eyes
- Smarting or burning eyes
- Eyes tire easily, particularly noticeable when reading, watching TV or using a computer
- Contact lens discomfort or intolerance
- Excessive mucus discharge
- Watery eyes
- Eyes easily irritated by smoke
- Sensitivity to light (photophobia)
- Fluctuating vision
- Blurred vision, particularly first thing in the morning and/or late in the day
- Eyelids ‘stick shut’ at night
- Eyelids feel ‘heavy’
Severity/Classification of Dry Eyes
Mild dry eye conditions can usually be managed satisfactorily with artificial tear supplements, lid therapy and other common treatments. Many millions of people may suffer from dry eyes from time to time and many will be unaware of the symptoms.
Moderate dry eye may affect vision more, and will probably affect quality of life a lot more because of chronic pain, eye sensitivity, light sensitivity and restricted activities.
Severe dry eye may lead to desiccation of the corneal epithelium, ulceration and perforation of the cornea, an increased incidence of infectious disease and, potentially, serious visual impairment and blindness.
More information about dry eyes severity is available on the DEWS Report 2007.
Epidemiology and causes
Dry eye syndrome has a higher prevalence amongst women and those over 60 years old; however, it is an extremely common eye condition and has a wide range of causes, including:
- Medical Conditions
- Systemic diseases (Sjogrens syndrome, RA (Rheumatoid Arthritis), Lupus erythematosus, Stevens Johnson, thyroid disease, Bell’s palsy)
- Eye conditions (ocular rosacea, corneal dystrophies)
- Rosacea
- Meibomian Gland Dysfunction (MGD)
- Eyelid conditions (lagophthalmos, ptosis)
- Eye injuries and burns
- Conditions of the eyelid, such as blepharitis
- Vitamin A deficiency
- Neurological lesions (e.g. Riley-Day syndrome)
- Absence/abnormality of lacrimal gland/ductules
- Idiopathic reasons
- Blink disorders
- Blepharitis anterior or posterior
- Ocular surface disease/allergic conjunctivitus
- Medications
- Systematic drug side effects (antihistamines, diuretics, beta blockers, HRT, oral contraceptives, selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs))
- Chemotherapy and radiation
- HRT
- Preservatives in topical treatments
- Surgery
- LASIK surgery
- Blepharoplasty
- Refractive surgery
- Biological factors
- Age
- Gender
- Hormonal (e.g menopause)
- Lifestyle factors
- Diet
- Lack of sleep
- Contact Lenses
- Prolonged computer use (or portabel devices with screens)
- Environmental
- Air conditioning, car heaters, air currents
- Smoky and dusty environments
- Air pressure changes (e.g. on a plane)
Diagnostic tests
Diagnosis
These are the tests most commonly used to diagnose dry eyes syndrome.
TEAR FILM STABILITY TESTS
Normal tear film is continuously available. Blinking maintains the tear film continuity. However if you keep your eyes open long enough, without blinking, the tear film will start breaking up. Your eye will feel uncomfortable forcing you to blink. In patients with dry eyes the tear film is unstable, and breaks up faster. Therefore the tear break up time in patients who have dry eyes is shorter.
- Tear Film break-up time (TFBUT or FBUT)
This measures the interval between the individual’s last complete blink and the break-up of his or her tear film
- This simple test involves the use of a slit-lamp, set on a bright light setting with a cobalt blue filter:
- Instil fluorescein into the lower fornix.
Ask the patient to blink several times and then stop. - Measure the time between the last blink and the first appearance of a dark spot on the cornea (formation of a dry area) on the otherwise continuously stained tear film.
A tear break-up time of less than 10 seconds suggests a dry eye.
- Non-invasive tear break up time (NIBUT)
In the F B U T test the presence of fluorescein in the tears may stimulate reflex tearing and may also result in changes to the tear film properties. To overcome these potential limitations, Non Invasive Break up time (NIBUT) methods have been developed. They are called “Non Invasive” because the eye is not touched.
- Instruments such as a Keratometer, hand-held Keratoscope or Tearscope are required to measure NIBUT.
- A pre-rupture phase that precedes actual break up of the tear film can also be observed with some techniques. This pre-rupture phase is termed Tear Thinning Time (TTT). Measurement is achieved by observing the distortion (TTT) and/or break up (NIBUT) of a keratometer mire (the reflected image of keratometer grid). The clinician focuses and views the crisp mires, and then records the time taken for the mire image to distort (TTT) and/or break up (NIBUT).
- NIBUT measurements are longer than fluorescein break up time. NIBUT values of less than 15 seconds are consistent with dry eyes.
TEAR VOLUME TESTS
Tear volume and production are components of tear film stability and can be affected by dry eye. One common method for determining tear volume is the Schirmer test.
- Schirmer test
- Instil a drop of local anaesthetic into the eye, (optional).
- Prepare a filter paper (5mm x 35mm with folded end).
- Gently dry the eye.
- Apply the filter paper with the folded end hooked onto the lower lid margin at the junction between the middle and outer third (take care not to touch the cornea).
- Tell patient to keep their eye open and blink normally.
- Measure the amount of wetting after 5 minutes: 13-15mm wetting rules out a dry eye; 6-10mm is borderline and less than 6mm indicates dry eye.
- The filter paper strips can cause reflex tearing and may require the use of anaesthetic agents. However, they still provide a measurable clinical indication of dry eye.
- Phenol Red Test
A cotton thread impregnated with phenol red dye is used. Phenol red is pH sensitive and changes from yellow to red when wetted by tears.
- The crimped end of a 70mm long thread is placed in the lower conjunctival fornix.
- After 15 seconds, the length of the colour change on the thread – indicating the length of the thread wetted by the tears -is measured in millimetres.
- Wetting lengths should normally be between 9mm and 20mm. Patients with dry eye have wetting values of less than 9mm.
- Tear Prism Height Test
A significant amount of information about tear quantity can be gained simply from observing the heights of the upper and lower tear menisci with the slit-lamp biomicroscope.
There are two techniques used when measuring the height of tear prisms. The first measures the tear meniscus formed on the lower lid margins to give a useful guide to tear volume. This simple technique employs the slit lamp biomicroscope. Excessive or prolonged use of illumination should be avoided to prevent artificial drying of the tear prism.
The second technique is to compare the tear prism height with the illuminated slit width by setting the slit horizontally in alignment with the lower lid margin, altering the slit width until it appears to match the height of the tear prism. Heights of less than 0.2mm indicate reduced tear fluid quantity.
Observation of the meniscus profile is also extremely helpful. A regular tear meniscus is typically observed in a healthy eye while a meniscus with a scalloped edge is often associated with a dry eye.
STAIN TESTS
Ocular staining serves as an indicator of the health of the ocular surface.
- Rose Bengal Test (No longer widely used)
End-organ damage to conjunctival and corneal epithelial cells can be assessed via Rose Bengal ocular surface staining, which identifies areas of devitalised tissue:
- Instill a drop of Rose Bengal dye into the inferior fornix of the unanesthetised eye.
- Ask the patient to blink twice, to spread the red stain over the conjunctiva and cornea.
- The ideal time to measure the presence of staining is approximately 3 to 5 minutes after instilling the drops.
- Score the staining using a slit-lamp: a pattern of exposure zone (interpalpebral) corneal and bulbar conjunctival staining is typically seen with aqueous tear deficiency.
- Lissamine Green
Lissamine green staining like Rose Bengal, colours any desiccated and dying cells on the ocular surface. However, lissamine green may be better accepted by patients as it lacks the slight burning or stinging sensation typically found with rose Bengal.
- Fluorescein
Fluorescein staining penetrates areas of the corneal epithelium and conjunctival epithelium where intercellular junctions are disrupted.
HYPEROSMOLARITY TEST
Hyperosmolarity of the tear film is recognized as an important pathogenetic factor in dry eye syndrome (DES). Tear hyperosmolarity may be regarded as the single feature that characterises the condition of “ocular surface dryness”.
Hyperosmolarity testing has been hampered in the past by difficulties in tear collection and analytic procedures that required laboratory facilities. Recently, ‘lab-ona- chip’ technology has enabled osmolarity measurement to reach the clinical setting.
The Tearlab Osmolarity System is a new user-friendly tool that only needs tiny volumes for analysis and determines hyperosmolarity semi-automatically.
The disposable probe, touched onto the lower tear meniscus at the lid margin, collects a nanolitre sample of tears, which is analysed within seconds to provide the clinician with an osmolarity reading. Normal values lie around 304mOsm/kg while values over 320mOsm/kg indicate dry eye.
Artificial tears and lubricants
The term ‘artificial tears’ is commonly used to describe drops, solutions and liquid gels applied directly into the eye. The term is not strictly correct, however, as artificial tears do not accurately mimic the composition of real tears – they mainly act as lubricants. The term ‘ocular lubricants’ generally refers to more viscous products such as ointments.
Mild or moderate dry eye symptoms
- Artificial tears alone are usually sufficient to provide relief
- Hypromellose is a widely used product, and can be administered frequently
- Products containing carbomers or polyvinyl alcohol are longer-acting
- Sodium chloride 0.9% is short acting and suitable as ‘comfort drops’
- Sodium Hyaluronate is becoming more widely used because of its water-retaining properties and low resistance to blinking
Some eye drops contain preservatives and can cause irritation. If someone is sensitive to preservatives or uses soft contact lenses, consider switching to one that is preservative-free. Carmellose sodium, hydroxyethylcellulose, carbomer, polyvinyl alcohol, hydroxypropyl guar, sodium hyaluronate, hypromellose and povidone are all available without preservatives.